If you have lung cancer and smoke, it is important to quit. Smoking can interfere with the way treatments work and can make side effects worse. Research has progressed and the discovery of different types of lung cancer has imaged. As we learn more about lung cancer we know that treatment options depend not just on the type but also the subtype and in some case gene mutations.
If you have lung cancer and smoke, it is important to quit. Smoking can interfere with the way treatments work and can make side effects worse. Research has progressed and the discovery of different types of lung cancer has imaged. As we learn more about lung cancer we know that treatment options depend not just on the type but also the subtype and in some case gene mutations.
Knowing what is available for treatment options will help you have an informed discussion with your doctor.
Second Opinions
If you have been told you have lung cancer getting a second opinion is always a good idea. Your physician should encourage you to explore other opinions. If he/she feels threatened by your decision you may want to rethink your relationship with that doctor. Getting a second opinion must be made before you enter treatment.
Surgery
Surgery to remove the tumor may be performed. Depending on where and how big the tumor is will depend on whether a small part of the lung (wedge resection or segmentectomy) is performed, removing a lobe of the lung (lobectomy or sleeve lobectomy) or removal of the entire lung (pneumonectomy).
Some questions you might want to ask your doctor might be:
What type of surgery will I have?
How will I feel after surgery?
How will I control my pain?
How long will I be in the hospital?
Will there be any lasting side effects?
When can I return to normal activities?
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It affects cells only in the treated area. Radiation can be given externally or internally (brachytherapy). Internal radiation is seldom performed on lung cancer patients. The side effects depend mainly on the type of radiation therapy, the dose level of radiation, and the part of your body that is treated. Radiation to the chest may harm the esophagus, causing problems with swallowing. You may feel tired and your skin may become red, dry and tender in the treated area.
Some questions you might want to ask your doctor:
Why do I need this treatment?
What kind of radiation therapy do I need?
When will the treatment begin and when will it end?
How will I feel during treatment?
How will you know if the radiation treatment is working?
Are there any long term side effects?
Chemotherapy
Chemotherapy is a treatment with chemicals that kills cells that divide or grow rapidly, like cancer cells. Usually, more than one drug is given. The drugs are administered through the vein. Some cancer drugs can be taken by mouth. The chemotherapy is given in cycles. You will have a rest period after each treatment. The length of the rest cycle and number of cycles depends on the cancer drugs used. The side effects depend on the type of drugs given. The drugs can harm normal cells that divide rapidly such as blood cells, cells in the hair root and cells that line the digestive tract. Treatment can lower the levels of healthy blood cells making you more likely to get infections, bruise or bleed easily. You may feel very weak and tired. You may lose all or part of your hair however the hair will grow back after treatment ends. It may be somewhat different in color and texture. Chemotherapy can cause poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Your physician can prescribe medication to help with this. Some drugs can cause hearing loss, joint pain, and tingling or numbness in your hands and feet. These side effects usually go away after treatment ends. When radiation and chemotherapy are given at the same time, the side effects may be worse.
Targeted Therapy
Researchers are discovering more about how lung cancer cells grow and spread. Just as each and every one of us is unique so are lung cancer cells.
What is targeted therapy?
Targeted therapies are drugs or other substances that block the growth and spread of cancer by interfering with specific molecules that have changed within the lung cancer and are involved in tumor growth and progression. By focusing on these molecular and cellular changes that are specific to the cancer cell, targeted therapies may be more effective than other types of treatment and less harmful to normal cells. This is different than traditional chemotherapies that work by killing any rapidly dividing cells in the body.
How do targeted therapies work?
Targeted therapies interfere with the way a cancer cell divides and spreads in different ways. Many of these therapies are directed against proteins that are involved in cell signaling pathways, which form a complex communication system that governs basic cellular functions and activities, such as cell division, cell movement, cell responses to specific external stimuli, and even cell death. By blocking signals that tell cancer cells to divide uncontrollably, invade and metastasize, targeted cancer therapies can help stop cancer progression and may induce cancer cell death through a process known as apoptosis. Other targeted therapies can cause cancer cell death directly, by specifically inducing apoptosis, or indirectly, by stimulating the immune system to recognize and destroy cancer cells and/or by delivering toxic substances directly to the cancer cells.
What test for targeted therapies are currently available?
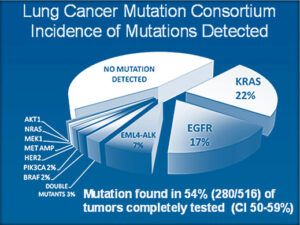
As you can see from the pie chart researchers have identified many gene mutations and alterations in lung cancer tumors. Thus far, effective treatments for them have not been developed for all mutations. Currently, there are three genes that are most frequently tested for lung cancer mutation. They are Epidermal Growth Factor Receptor (EGFR), Anaplastic Lymphoma Kinase (ALK), and Kirsten-ras (Kras).
How are these mutations identified?
These mutations are identified by studying samples of tissues from the lung cancer patient. The procedure to obtain tissue samples can be conducted through bronchoscopy, mediastinoscopy, lymph node biopsy, CT guided CORE needle biopsy and via VATS (Video-assisted thoracoscopic surgery procedure). Because this is a relatively new procedure it is important that your physician is familiar with tumor testing and targeted therapy. It is always recommended and advisable to get a second opinion from a highly informed thoracic oncologist familiar with these changes and targeted therapies.
What therapies are currently available?
While several targeted therapies have already been approved for use in lung cancer, many more have been identified as possible treatments and are being tested in clinical trials. Here are just a few:
Epidermal growth factor receptor (EGFR) mutation-positive tumors are likely to be sensitive to drugs like Tarceva. Tarceva is an EGFR inhibitor. It is taken in pill form. This drug may cause cancer to stay dormant or even disappear for a long time. Its side effects are less invasive than traditional chemotherapy, radiation, and surgery. Side effects may include diarrhea and skin rash.
Anaplastic Lymphoma Kinase (ALK) positive tumors respond well to a new drug like Crizotinib (Zalkori) which is an ALK inhibitor. This drug is also taken orally. This drug is only available in clinical trials. This small-molecule drug inhibits the tyrosine kinase activity of a fusion protein called EML4-ALK, resulting in decreased tumor cell growth, migration, and invasiveness. It appears to have mild side effects in the clinical trial.
For Kirsten-ras (Kras) mutation positive tumors there are no therapies at present, however, there are many clinical trials.
Depending on your unique situation, your doctor may recommend one or multiple of the following approved drugs:
Drugs Approved for Non-Small Cell Lung Cancer
- Abraxane (Paclitaxel Albumin-stabilized Nanoparticle Formulation)
- Afatinib Dimaleate
- Afinitor (Everolimus)
- Alecensa (Alectinib)
- Alectinib
- Alimta (Pemetrexed Disodium)
- Alunbrig (Brigatinib)
- Atezolizumab
- Avastin (Bevacizumab)
- Bevacizumab
- Brigatinib
- Carboplatin
- Ceritinib
- Crizotinib
- Cyramza (Ramucirumab)
- Dabrafenib
- Dacomitinib
- Docetaxel
- Durvalumab
- Erlotinib Hydrochloride
- Everolimus
- Gefitinib
- Gilotrif (Afatinib Dimaleate)
- Gemcitabine Hydrochloride
- Gemzar (Gemcitabine Hydrochloride)
- Imfinzi (Durvalumab)
- Iressa (Gefitinib)
- Keytruda (Pembrolizumab)
- Lorbrena (Lorlatinib)
- Lorlatinib
- Mechlorethamine Hydrochloride
- Mekinist (Trametinib)
- Methotrexate
- Mustargen (Mechlorethamine Hydrochloride)
- Navelbine (Vinorelbine Tartrate)
- Necitumumab
- Nivolumab
- Opdivo (Nivolumab)
- Osimertinib
- Paclitaxel
- Paclitaxel Albumin-stabilized Nanoparticle Formulation
- Paraplat (Carboplatin)
- Paraplatin (Carboplatin)
- Pembrolizumab
- Pemetrexed Disodium
- Portrazza (Necitumumab)
- Ramucirumab
- Tafinlar (Dabrafenib)
- Tagrisso (Osimertinib)
- Tarceva (Erlotinib Hydrochloride)
- Taxol (Paclitaxel)
- Taxotere (Docetaxel)
- Tecentriq (Atezolizumab)
- Trametinib
- Trexall (Methotrexate)
- Vizimpro (Dacomitinib)
- Vinorelbine Tartrate
- Xalkori (Crizotinib)
- Zykadia (Ceritinib)
Drug Combinations Used to Treat Non-Small Cell Lung Cancer
Drugs Approved for Small Cell Lung Cancer
- Afinitor (Everolimus)
- Doxorubicin Hydrochloride
- Etopophos (Etoposide Phosphate)
- Etoposide
- Etoposide Phosphate
- Everolimus
- Hycamtin (Topotecan Hydrochloride)
- Mechlorethamine Hydrochloride
- Methotrexate
- Mustargen (Mechlorethamine Hydrochloride)
- Nivolumab
- Opdivo (Nivolumab)
- Topotecan Hydrochloride
- Trexall (Methotrexate)
National Cancer Institute at the National Institutes of Health
Vanderbilt-Ingram Cancer Center
My Cancer Genome Overview of Targeted Therapies
Chemoprevention
The term “chemoprevention” refers to efforts to prevent or delay the development of lung cancer by taking medicines, vitamins or other agents. There are many trials being studied but have not shown anything certain thus far. One, in particular, is Celecoxib (Celebrex) an anti-inflammatory drug used to block the pain caused by arthritis by blocking an inflammation-causing chemical called COX-2.
Early Detection
Lung cancer is so difficult to treat is because it is often found after it has spread to other parts of the body. Unfortunately, there are no early symptoms. The National Lung Screening Trial (NLST) study showed that low dose chest CT scans to screen those at high risk for lung cancer reduced the number of lung cancer deaths by 20%. You can review the study at screenforlungcancer.org. There are several other studies being conducted to detect early-stage lung cancer. Some of those include blood tests, breath tests, sputum cytology and cell sampling from the airway via bronchoscopy. Unfortunately, these tests have not been approved and are still being studied.